ARCHIVED FREE CHRONIC PAIN ARTICLES

Relapse Prevention Planning Is Crucial For Chronic Pain Management
This Article Relapse Prevention Planning Is Crucial For Chronic Pain Management With Coexisting Substance Use Disorders, was first published on RecoveryView.com, an Online Journal on June 4, 2020.
Clearly Defining Relapse Is Crucial
If you ask someone in the medical field about relapse, they most likely will say relapse is going back to an active state of a disease after a period of remission. When you ask someone recovering from inappropriate use of medications, including using alcohol or other drugs they may say it’s going back to using the substance again.
While that definition is partially correct, it can be dangerous, especially if people thinks the only criteria for recovery is abstinence. Another common definition of relapse is that a person goes back to their addiction process. The full explanation of relapse is much more complex and must include not only maintaining abstinence or an appropriate medication management plan but also stop following their mental health treatment plan or sabotaging their chronic pain management plan.
- People can head back towards relapse without even thinking of using
- They can start sabotaging their effective chronic pain management plan
- People also stop following their mental health treatment plan
What many people don’t realize is that the chemical use or coming out of remission is not the beginning of a relapse. It is the final step in an ongoing relapse process. In addition, relapse is a common symptom of a medication use disorder or other chemical use disorders, and one-third to two-thirds of all recovering people in chemical recovery relapse despite their best intentions not to do so. The good news is we can take the mystery out of relapse and increase people’s chances for positive recovery without a chemical relapse episode.
If someone is also living with a coexisting disorder—e.g., chronic pain, depression, PTSD or an anxiety disorder—the instance of relapse can be even higher because these other problems can easily become relapse justifications. Fortunately, the risk of relapse can be lowered if recovering people are exposed to education and training about relapse prevention and how to deal more effectively with all of their coexisting problems. Prevention is much easier than crisis management.
Relapse is the process of becoming dysfunctional in your recovery!
I believe relapse education must start with a new definition of relapse. The definition I propose and share with my patients is: Relapse is the process of becoming dysfunctional in your recovery process. Relapse is a progressive series of events that takes people from a stable recovery through various stages of dysfunction, and eventually go back to using inappropriate medications, alcohol or their other drugs of abuse.
I tell my patients that when you start on the slide to relapse you will undergo many changes. One of the first changes is a return to denial that at first has nothing to do with substance use, sabotaging your pain management plan or addictive behaviors. In other words, you begin denying that you need to work a program of responsible living, healthy communication with others, and constantly looking at yourself for evidence of progress and problems in yourself and your life. To deny these needs leads to thinking problems.
Now instead of responsible recovery-prone positive thinking people start experiencing relapse-prone negative thinking and eventually euphoric recall. This negative thinking leads to experiencing uncomfortable and/or painful emotions. These feelings produce self-defeating urges which are often followed by self-destructive behaviors or ineffective chronic pain management. Inappropriate use of medications, alcohol or other drugs may not be an option in the early stages of relapse, but the negative behaviors often set people up to experience even more problems including increased pain flare ups.
To request the remainder of this article, please connect with me at drgrinstead@yahoo.com.
Moving Beyond Anticipatory Pain for Effective Pain Management
If you’re living with a chronic pain condition like I am you may have noticed that sometimes you are so fearful about doing even the most basic tasks of daily living, that you become immobilized. It can also manifest as overwhelming anxiety, so much so, that a phenomenon gets triggered which amplifies your perception of pain. I call this Anticipatory Pain.
Because you believe you are going to hurt by doing a certain activity, you can activate the physical pain system. Just by thinking about doing something that you believe will cause you to hurt, you will start to feel pain. This can happen before you even do whatever it is you already believe will cause physical pain. All you have to do is to start thinking about doing that thing.
Once the physical pain system is activated, the anticipatory pain reaction can make your perception of chronic pain symptoms worse.
Whenever you feel the pain, you interpret it in a way that makes it feel worse, and you think about it in a way that actually does make it worse. You tell yourself that “this pain is awful and terrible,” and “I can’t handle it.” You convince yourself that “it’s hopeless, I’ll always hurt, and there’s nothing I can do about it.”
This way of thinking contributes to the development of emotional reactions that further intensify or amplify the pain response. The increased perception of pain causes you to keep changing your behavior in ways that create even more unnecessary limitations and mounting emotional discomfort. These reactions can make you believe you are trapped in a progressive cycle of disability.
Coping and Moving Beyond Anticipatory Pain
One of the most requested articles I wrote was titled “Coping with Anticipatory Pain. I believe it’s vital for us to support people to not just cope with anticipatory pain, but to move beyond it.
I learned a long time ago that what we expect is usually what we get which can sometimes be both helpful and harmful. When it comes to feeling pain and developing an effective chronic pain management plan, it’s crucial to understand the role of anticipatory pain. It has both biological and psychological components.
On the biological side, the cascade of effects from a pain sensation occurs on many levels and involves a variety of different areas within the nervous system. As a result, a wide variety of nervous system chemicals are produced and dumped into the blood while other brain chemicals are rapidly absorbed or depleted. Pain doesn’t just hurt — it changes the most basic neurophysiologic processes in the human body.
On the psychological side, anticipation of an expected pain level can influence the degree to which you experience your pain. In some cases, when your anticipatory level of pain expectation is lowered, your brain responds by influencing special neurons. This renders your brain less responsive to an incoming pain signal and your sensation of pain decreases. In any event, both ascending (pain signals coming from the point of injury to the brain) and descending nerve pathways (signals from the brain to the point of injury) will influence or modify the effects on your body.
To request the remainder of this article, please connect with me at drgrinstead@yahoo.com.
The Role of Spirituality in Chronic Pain Management Is Crucial
Chronic pain is often misunderstood and undertreated. In addition to the biopsychosocial impact a chronic pain condition frequently has on a person, a spiritual crisis often accompanies the situation as well. Long-term chronic pain is a body-mind-spiritual problem that requires a multifaceted solution. I believe that complementary spiritual practices are necessary components of any effective chronic pain management plan.
Many people have found spiritual interventions like the traditions of prayer and meditation to contribute to the reduction of the sense of suffering. Unfortunately, in our fast-paced world and the secular treatment modality, adding a spiritual component to chronic pain management does not get enough attention.
The concept of spiritual pain requires healthcare providers to go beyond the bounds of traditional clinical treatments and be prepared to devote the time required to give supportive and understanding care. It is crucial to explore spirituality and its impact on a person’s pain in a multidimensional assessment.
It’s Time To Think Outside The Box
Spirituality is vital aspect of being human which is difficult to fully understand or measure using scientific methods; yet convincing evidence in medical literature supports its beneficial role in the practice of medicine. It will take many more years of study to understand exactly which aspects of spirituality hold the most benefit for health and well-being.
Many of the world's great wisdom traditions suggest that some of the most important aspects of spirituality lie in the sense of connection, inner strength, comfort, love and peace that individuals derive from their relationship with self, others, nature and the transcendent.
I believe that spiritual healing is an important component of a multifaceted chronic pain treatment plan. One goal of spiritual healing is to help patients improve their well-being and quality of life, rather than to cure specific diseases or in this case eliminate pain. Spirituality as part of a treatment plan may include encouraging patients to use visualization, prayer and positive thinking.
The Difference Between Religion and Spirituality
Over the years I have found it important to have a discussion with my patients regarding spirituality and effective pain management, as a common understanding of terminology is essential as is an understanding of what their beliefs are.
One concept that rang true was the simple saying: “Religion prepares people for the next life while spirituality helps them live this life to their fullest potential.” Many of my colleagues also recommend clarifying the difference between the terms “spirituality” and “religion.” They advocate developing a broad-based definition of spirituality that encompasses religious and nonreligious perspectives.
To request the remainder of this article, please connect with me at drgrinstead@yahoo.com.

Chronic Pain Management and the Impact on Family and Friends
The Family Also Needs A Bio-Psycho-Social-Spiritual Approach To Heal
I’m writing this for people who are living with someone—or care for someone—who is suffering with a chronic pain condition and they are having a hard time coping because they’re not sure how to help. Unless someone’s been in your place they have no idea how challenging this can really be.
I’ve seen many marriages and partnerships end due to one of the partners living with an undertreated or mistreated chronic pain condition. Sometimes family members and significant others develop their own healthcare problems while trying to help someone they love cope with chronic pain. Family and significant others often get burned out, or they become frustrated and resentful towards the person living with chronic pain. A spouse can become just as hopeless and helpless as their family member who is suffering with pain and may even develop a severe depression or sleep problem.
For those of you helping someone living with a chronic pain condition who don’t have a personal experience of living with chronic pain I want to ask you to follow the steps below to see if you can develop a better understanding of what it must be like to live with chronic pain. To get the most out of this following exercise please make sure to do it when you have the time and space where you won’t be interrupted. It’s also helpful if you journal your reactions to this as soon as you’ve completed the four steps below.
Step One: Think back to a time when you hurt yourself or had a painful condition such as a surgery, toothache, broken bone, or headache etc.
Step Two: Try to remember what that felt like and what you wanted to do to stop the pain.
Step Three: Now imagine that you have that level of pain right now and have had it for the past six months without any relief. Every day when you woke up it was there. Every night you wonder if you’ll be able to sleep because the pain is so disturbing.
Step Four: Now imagine trying to explain this to your family and friends or your healthcare provider. What would you say? What would you want from them? Please make sure write down your reactions to this brief exercise.
What kind of healthy support can friends and family provide if a loved one is undergoing chronic pain management, experiencing significant quality of life problems and a decreased level of functioning? The most important thing is to understand what it must be like; if you answered the four questions above and reflected on what you learned, you should have a much better idea.
Here are six additional starting points.
1. Make sure that you are practicing good self-care; take time to relax, sleep, play, eat healthy, etc.
2. Develop compassion and even empathy for your significant other—but never sympathy as that can cause even more problems. Remember the old saying “Sympathy Kills” that is often heard at Al-Anon meetings.
3. Do NOT do things for your significant other that they can and should be doing for themselves.
4. Don’t keep secrets from your significant other. This is especially true concerning medication use or abuse issues.
5. Remember the three (3) Cs of Al-Anon: You didn’t CAUSE it, you can’t CONTROL it, and you can’t CURE it.
6. Seek out a professional with experience in chronic pain and any coexisting problems for you and your family.
However, these are just starting points. In order to help someone else, you first must make sure to take care of yourself. You also need to be aware of the two major traps—enabling and resentment. Enabling is when you find yourself doing something for your friend or loved one that they can and should be doing for themselves.
When supporting someone living with chronic pain for long periods of time many people are at risk of burnout. What started as loving care and support sometimes turns into a major chore and the helper becomes angry and resentful of the person living with chronic pain. Just like many people who are living with chronic pain become isolated and depressed; many helpers also fall into these problems.
To request the remainder of this article, please connect with me at drgrinstead@yahoo.com
Effective Chronic Pain Management is a Right and a Responsibility
People living with an ongoing chronic pain condition often give up trying to explain to their healthcare providers or even loved ones, what living with pain is like! They get tired and frustrated of being told it’s all in their head, that they’re malingering, drug seeking, or that they just need to learn to live with it.
Then there are some people who try to seek help, but sometimes in ways that are not in their best interest. Others are on a quest to find the magic solution: the right pill, procedure, healthcare provider or technique that will give them the relief they want, or some kind of plan that will just stop the pain. They get fixated on the traditional Bio-Medical Model and for many it is not very effective as it often fails to identify and/or treat the coexisting psychological and medication use problems often occurring with people suffering with chronic pain.
First of all, there is nothing wrong with wanting pain relief. However, it may be unrealistic for some people with certain pain conditions to ever be pain free. In this instance I ask my patients: even if you had a certain level of pain, would it be all right if you never had to suffer with it again? This is why I wrote the book Thank You Adversity For Yet Another Test.
In fact, I often have to apply the information I write about to myself. Especially when I was recently experiencing acute pain flare ups that could keep me in bed, unable to work or participate in normal activities. For many years I have been dealing with my own chronic pain condition, but it had several decades since I felt this kind of intense pain. It would have been easy to obsess about my pain and become depressed as a result.
I almost slipped back into what I call the “chronic pain trance,” which is a state of mind that develops when someone has to live with pain on a daily basis over a long period of time. What is important to remember is that this state is an automatic and unconscious way of coping with chronic pain which can be self-defeating or sometimes even self-destructive. Fortunately, I did start to practice what I teach.
Developing A Positive Relationship With Your Pain Is Crucial
When working with patients, I ask them to examine their personal relationship with pain and how they currently manage it, as well as taking an honest look at their medication management plan. The more proactive people are, the more they will improve their ability to manage their pain condition. But no one has to take this journey alone. I encourage my patients to share their journey with the people who care about them so they can understand more about what it takes to cope with a challenging pain condition.
People living with chronic pain that are ready to, can learn how to more effectively manage it, end their suffering, and improve their quality of life. But here is the challenge—effective pain management is not only a right, it is also a responsibility. Patients must take responsibility for their health and healing. In fact, they are the only ones that can. The challenge is to help them decide if they are willing to do the work required for effective chronic pain management and to become free from suffering.
One important suggestion for anyone living with chronic pain is to stop making pain the enemy. This can be a challenge, but is nonetheless a crucial first step. When I talk to patients about living with chronic pain, I often hear statements such as “I have a bad knee” or “this stupid pain is killing me.” These types of statements make clear to me that this person is still at war with their pain. Unfortunately, this is an internal war — one that cannot be won through fighting it.
People have to stop fighting their pain and make peace with it—pain is a part of who we are, so we are really just fighting with ourselves. When we make peace with our pain and learn how to manage it more effectively, we stop suffering. We become empowered to create a life worth living filled with meaning and satisfaction. However, in order to make peace with our pain, we need to move beyond the “quick fix.”
Effective Chronic Pain Management is NOT a Quick Fix
To request the remainder of this article, please connect with me at drgrinstead@yahoo.com.
Defining Effective Chronic Pain Management
Given the biopsychosocial nature of chronic pain conditions it is imperative to utilize a multidisciplinary treatment plan for effective pain management. Living with chronic pain is very difficult. If you also have a coexisting addiction or other psychological conditions, it becomes even more challenging. People with chronic pain and coexisting disorders can become severely depressed and feel hopeless. Their self-esteem is practically non-existent and many of them lose the support of their significant others.
Healthcare providers often become confused and frustrated when their treatment interventions are ineffective. Also, people living with chronic pain must educate themselves and be proactive consumers regarding health practitioners who claim to do pain management. Be wary, if they offer only one type of modality for addressing your pain, such as medication management, or chiropractic adjustments or acupuncture.
True multidisciplinary pain management involves interventions such as physical therapy, massage, medication management, counseling or therapy, biofeedback, occupational therapy, exercise physiology, an anesthesiologist or pharmacologist, and a case manager all at one site, at a minimum. It may also involve some type of movement therapy such as Tai Chi, classes on spiritual wellness, yoga or meditation.
Success Requires A Team Approach
In my experience, a multidisciplinary team is crucial in order to address the specific biopsychosocial needs of people living with chronic pain. In addition, the physical, psychological, and social implications of chronic pain and any coexisting condition—including the impact on family systems—must also be adequately dealt with.
Using a multidisciplinary team is crucial when treating the synergistic problems people and their families’ face that have been severely impacted by chronic pain, especially when addiction and other psychological problems are present. When these conditions coexist it creates a major challenge that must be addressed through a collaborative treatment approach. The inclusion of addiction, mental health and medical is vital to this process.
When these coexisting conditions occur, the family problems increase synergistically. Effective treatment can be challenging and confusing for counselors, therapists and other healthcare providers, but especially for patients and their families. I have found that the strategic three-part approach mentioned in last month’s article improves treatment outcomes and gives people living with chronic pain and their families new hope.
To request the remainder of this article, please connect with me at drgrinstead@yahoo.com
Identifying Red Flags For Pain Medication Problems
I developed the information in this article to help my patients take a look at their relationship with medications. Differentiating between appropriate use of psychoactive medications with abuse or addiction potential and the beginning of abuse can sometimes be difficult for patients and their healthcare providers to determine. Some medications also have the potential for problematic use including medication dependency, medication abuse, pseudo-addiction, and finally addiction. The confusion and uncertainty of this progression can be challenging for everyone.
The Benefits and Risks of Using Medication
The benefits of medicines are the helpful outcomes people get when they use them, such as lowering blood pressure, curing infection or relieving pain. The risksof medicines are the chances that something unwanted or unexpected could happen to people when they use them. Risks could be less serious things, such as an upset stomach, or more serious things, such as liver damage or even addiction.
When a medicine’s benefits outweigh its known risks, The U.S. Food and Drug Administration (FDA) consider it safe enough to approve. But before using any medicine—as with many things that people do every day—people should be clear about what those benefits and risks are in order to make the best choices.
Some of the Risks from Medication Use
- The possibility of a harmful interaction between the medicine and a food, beverage, dietary supplement (including vitamins and herbals), or another medicine. Combinations of these products can increase the chance of interactions.
- The chance that the medicine may not work as expected.
- The possibility that the medicine may cause additional problems.
Every choice to take a medicine involves thinking through the helpful effects, as well as the possible unwanted effects. The best choice depends on someone’s personal situation. People must decide what risks people can and will accept in order to get the benefits you want. For example, if facing a life-threatening illness, people might choose to accept more risk in the hope of getting the benefits of a cure or living a longer life.
On the other hand, if people are facing a minor illness, they might decide that they want to take very little risk. I always encourage my patients to think it through and work together with their healthcare team to better manage the benefits and risks of their medicines.
Weighing the Risks—Making the Choice
Directions: The benefit/risk decision is sometimes difficult to make. The best choice depends on a person’s particular situation. People must decide what risks they can and will accept in order to get the benefits they want. In many situations, the expert advice of peoples’ doctor, pharmacist, or other health care professional can assist them making the safest decision. Now please review the table below for some specific ways to lower the risks and obtain the full benefit from your medications.
To request the remainder of this article, please connect with me at drgrinstead@yahoo.com.

The New Rules for Treating Chronic Pain
Addiction-Free Solutions In The Era of Opioid Crisis
Prolog
These past years of COVID-19 have changed the face of healthcare in many ways; some positive and some extremely negative. There have been many casualties of COVID-19 above and beyond those living and dying with the exposure to this disease. Some of those casualties are people with chronic pain and coexisting disorders including addiction, PTSD, Depression, Anxiety and many other mental health problems. The other noted victims are people dying from Opiate/Opioid overdoses, in many cases due to not receiving adequate treatment interventions by their healthcare providers. Because of COVID-19 we have lost focus on the so-called Opioid Epidemic. This article outlines some of the overwhelming problems that led to what I am calling the Opioid and Chronic Pain Syndemic. Then I outline the need for implementing a synergistic solution that needs to include everyone. I am also including two case study examples to demonstrate the need and effectiveness of an Addiction-Free Pain Management® synergistic treatment solution.
Understanding the Problem is Crucial to Finding the Solution
I believe there is much more than an opioid crisis or epidemic. It is not an epidemic, rather it is a Syndemic. What I mean by that is it’s a perfect storm of over prescribing opioids, mismanaged chronic pain by depending only on the traditional bio-medical model and untreated mental health disorders. What we need to focus on is identifying the synergistic nature of the problem and the need to implement a synergistic treatment solution that helps heal the whole person – Biological, Psychological, Family/Social and Spiritual. A true Body-Mind-Spirit Approach.
There is also a strong political and financial component to our current problem that Harry Nelson outlines so well in his book The United States of Opioids: A Prescription For Liberating A Nation In Pain. Also, in his book Dreamland: The True Tale of America's Opiate Epidemic, Sam Quinones also covers some of the financial and political precursors to our current problem.
In addition, many people believe what underlies this crisis is a severe deficit in coping skills for those who are suffering with chronic pain and coexisting mental health disorders including substance use disorders. Combine these poor coping skills with misinformation from leading medical prescribers using opioids for chronic pain, and we see addiction from prescription opioids has increased over 1,000 percent between 2012 and 2016. The Center For Disease Control (CDC) posted an update on December 16, 2016 with some other staggering statistics:
- Over 1,000 people a day are being treated for prescription opioid overdose incidents with the three most common being Methadone, Oxycodone/OxyContin, and Hydrocodone.
- As many as 91 people a day are dying from prescription opioid overdose events.
- Between 1999 and 2015 there were over 183,000 deaths directly related to prescription opiates.
- Finally, in 2014 over 2 Million Americans experienced prescription medication misuse, abuse, pseudoaddiction or addiction. Many say this is an opioid epidemic.
The other coexisting epidemic noted is chronic pain. Chronic pain management is a serious health crisis facing the world today. In fact, in the well-publicized June 2011 White Paper The Institute of Medicine (IOM) stated that as many as 116 million people were experiencing chronic pain; the cost of managing it in the United States alone is over $635 Billion per year in direct medical costs and lost productivity. As I write this today the problem continues to worsen.
When a person who is undergoing chronic pain management, they are also experiencing other co-existing disorders, such as medication abuse or even addiction to prescription pain medication and psychological disorders, the problem reaches even more epidemic proportions. Every week in the media there are reports about the problematic use and/or abuse of prescription drugs being used in the treatment of chronic pain. The numbers of people impacted are staggering.
So what is the source of the so-called Opioid Epidemic and is there a link to chronic pain? A study posted in the New England Journal of Medicine in March of 2016, reported some interesting numbers in answer to this question.
More than 30 percent of Americans have some form of acute or chronic pain and among older adults; the prevalence of chronic pain is more than 40 percent. In 2014 alone, U.S. retail pharmacies dispensed more than 245 million prescriptions for opioid pain relievers. Opioids are widely diverted and improperly used. In addition, many physicians admit that they are not confident about how to prescribe opioids safely.
This report went on to state that more than a third (37 percent) of the 44,000 drug-overdose deaths that were reported in 2013 were attributable to pharmaceutical opioids while Heroin accounted for an additional 19 percent. There was also a parallel increase in the rate of opioid addiction, affecting approximately 2.5 million adults in 2014.
Alterations in brain functioning from living with chronic pain explains why long-term pain leads to cognitive deficits, as well as anxiety and depressive disorders. Emotional and cognitive deficits sometimes begin long after the onset of pain. Long-term pain may be detrimental to the brain and decrease the ability to endogenously control the pain and frequently lead to many comorbidities. (Neuroscience: 14: July 2013).
Unfortunately, the research numbers do not come close to capturing the true cost of the human pain and suffering experienced by those individuals with addiction whose pain condition is either under-treated or mistreated. When you add in the impact on families, friends and communities, it becomes even more devastating.
On September 16, 2016, Time Magazine came out with a report about why chronic pain patients turned to Heroin and the catastrophic results. The report stated that Heroin-related overdoses have almost quadrupled over the last decade in the U.S., leading to more than 10,000 deaths in 2014 alone. Heroin is being laced with Fentanyl and Carfentanil, two powerful synthetic opiates that are linked to a string of overdoses in the Midwest and Appalachia. In addition, since that time it has spread all across the nation.
A CNN Report on June 2, 2016 stated that today’s typical heroin addict starts using at age 23, is more likely to live in the affluent suburbs and was likely unwittingly led to heroin through the use of painkillers prescribed by his or her doctor. While heroin is illicit and opioid pills such as oxycontin are FDA-approved, each is derived from the poppy plant. Their chemical structures are highly similar, and they bind to the same group of receptors in the brain.
The FAIR Health, Inc. White Paper, in September 2016, covered the negative impact of the Opioid epidemic on healthcare. It showed the cost for opioid-related treatment rose over 1,000 percent from 2011 to 2015. It also stated that in 2015 Private Payers’ average costs for a patient diagnosed with opioid abuse or dependence were more than 550 percent higher than the per-patient average cost based on all patients’ claims and Emergency Room visits made up a large percentage of these costs.
The FAIR Health report went on to state that the bio-medical approach alone clearly doesn’t work for this poor outcome subset of chronic pain patients with coexisting disorder who end up over-utilizing the healthcare system and experience disappointing outcomes. So what does work? Now we are ready to get out of the problem and into the solution.
Investigating Potential Synergistic Solutions
In looking at potential solutions I’d like to review the cases of two of my former patients; the first, Patient One, is an excellent example of what can happen when a chronic pain condition is not managed appropriately and treatment depends only on medication-one part of the Biomedical approach.
To request the remainder of this article, please connect with me at drgrinstead@yahoo.com.
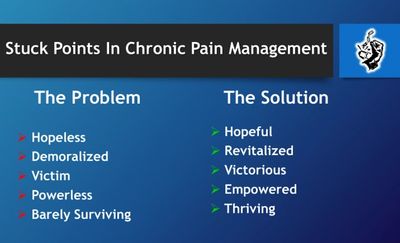
Identifying and Managing Five Stuck Points In Chronic Pain
Identifying The Obstacles
When confronted with issues that get in the way of effective chronic pain management, it is important to not linger too long in any phase of the healing continuum. Over the years I’ve seen many of my patients stop making progress and not transition through the following five phases.
- Hopeless to Hopeful
- Demoralized to Revitalized
- Victim to Victorious
- Powerless to Empowered
- Surviving to Thriving
In the sections below you will see the problem side of each transition point and the importance of moving through to a solution. Some of you may see where you have been or are currently stuck and need to move forward!
Out Of The Problem And Into The Solution
A point to remember is that the process is different for each person. Some people never experience any of these stuck points, while others may hit them all. Some of you may hit one or two or even three or four. That is why it is so important to understand the potential obstacles that can get in your way, and how, once you identify any one of them, you can then learn how to manage them by taking action and creating positive solutions.
Hopeless to Hopeful
Have you ever felt hopeless and helpless living with a chronic pain condition? If so, take yourself back to that time when you felt afraid and overwhelmed with a sense of hopelessness. Remember how that state of mind seemed to drain all of your energy along with hope for your future.
One of my patients, Sheena, had a workplace accident. She broke several bones and discovered over a year later that she also had severe nerve damage. Her doctors tried various pain medications and physical therapy interventions that first year. She kept trying to return to work as a carpenter, but ended up in so much pain that she had to stop working completely. She finally went on total disability and was told she would have to learn to live with the pain. Unfortunately, they did not explain to her how to do that and still have a functional, good quality of life.
Eventually she was referred to a pain clinic that I was consulting with. I worked with Sheena and her doctors to find out why nothing up to then had helped her pain. As I assessed her symptoms I noticed that nine of fifteen were neuropathic. I also discovered that she never received an MRI for her back; those results showed significant nerve impingements and damage.
Just know what was really going on was the beginning of Sheena’s transition from feeling hopeless to renewing a sense of hope for her future. Within six months she had adequate pain relief and was undergoing vocational rehabilitation in computer programming. Sheena was now very excited about her future, but without a healthy transition she would have been at high risk for getting stuck at the next transition: Demoralization.
Demoralized to Revitalized
When you get to the point of demoralization you may be at risk of wanting to quit or give up. At this point many people sink into a pit of depression that may lead to suicidal thoughts and even suicide attempts. This I what happened to one of my former patients, Jim.
Jim had been on total disability for over seven years when I first met him. He was referred to me after completing a mandated stay at a psychiatric hospital for an attempted suicide. At this point he was heavily medicated with antidepressants and other mood stabilizing psychiatric medications. His depression was still moderate to severe and he reported pain levels of 9-10 on a 0 to 10 pain scale on bad days and only 7-8 on his best days, even with his pain medication.
Our first step was for him to meet with a pain management colleague and to start on a medication that would address both his depression and pain symptoms.
As part of the solution Jim's doctor chose Duloxetine due to Jim’s significant neuropathic pain symptoms. I helped Jim develop a cognitive behavioral plan and within a few months he made the transition from demoralized to revitalized and felt as though he had his life back.
When people stay too long in a demoralized state, they often move to the victim stage. In this phase people can alienate and/or burn out friends and family. They are also at high risk for shifting back into hopelessness yet again.
To request the remainder of this article, please connect with me at drgrinstead@yahoo.com
Reevaluating The Bio-Medical Model
Over the past two decades I have seen that we as a nation have fallen victim to being sold the power of the pure bio-medical model for chronic pain treatment. Even though many research projects have all concluded that ethically, and for better outcomes, effective chronic pain management requires an integrated team approach.
Many chronic pain patients have been denied integrated services with the payors saying that there is not enough research to validate paying for these services.
However, this is not true. In fact, the truth is that there is no level one double blind research that demonstrates opioids are effective for chronic pain management.
There are, however, many evidence-based and research-based studies that demonstrate that integrated services such as Cognitive Behavioral Therapy, Acupuncture, Equine Therapy and many others can demonstrate improved outcomes for chronic pain patients. Despite this insurance companies have authorized thousands upon thousands of opioid prescriptions that eventually led to the dire problem we are experiencing today including thousands of overdose deaths all around the United States.
Defining The Bio-Medical Model
Part of the big picture is that opioids have proven very effective for acute pain management, such as broken bones, cuts, surgical procedures etc. Many big companies spent a lot of money and produced credible outcome research that demonstrated opioids we're effective for treating acute pain.
Some of the same big pharmaceutical companies spent millions of dollars if not more to tout using powerful opioids for chronic pain management. In one instance they purchased the right in the Journal of the American Medical Association to have the line OxyContin is not addictive, inserted. This along with the efforts of several high-powered medical doctors toured the country stating that it was a right for patience to have their chronic pain treated with opioids. At one point they spearheaded the movement to declare pain as the Fifth Vital Sign.
During the 1990s we started to see the growth of pain clinics cropping up all over the country. Pain clinics became a very lucrative business for many physicians especially anesthesiologists. In simple terms the bio-medical model became a combination of pills, injections, interventional pain procedures and surgeries. This model did seem to work very well for many pain patients. Unfortunately, for over 20 percent of the population showed little or no improvement with this model. Unfortunately, in many instances the patient was blamed for it not working.
There are many reasons why this 20 percent group of patients started over-utilizing most of the chronic pain healthcare dollars (some research shows as high as 80 percent) and they still showed little or no improvement. Why is that? The answer is complex, but I will attempt to share why I believe this occurs.
To request the remainder of this article, please connect with me at drgrinstead@yahoo.com.
Strategic Empowerment Pain Journaling Made Easy
I would like to share with you a valuable tool that I have developed and used with many of my chronic pain patients, as well as using it myself, over the past several years. In the remainder of this article I’m presenting the same education information and actual worksheets that I use with my patients.
Purpose Of Journaling About Pain
When I explain this process to my patients I start with the following directions: You are about to embark on a very personal and exciting journey. The Following information contains guidance for completing your personalized empowerment pain journal which will give you the power to begin making peace with your pain, allowing you to come to understand yourself on an intimate and powerful level. Believe that you have the ability to make your pain your friend! You have the power to utilize your pain as a loving guide that will direct you on your path of happiness and peace.
Your pain wants to teach and guide you! Your pain can show you how to nurture yourself, how to recognize unhealthy situations, to give you the insight to create a life of love and meaning. This journal will allow you the means to gain awareness and insights into the hidden messages your pain wants to communicate. As you uncover the hidden communication within your own personal pain cycles, you will gain a new sense of freedom and empowerment.
Goal Of Journaling About Pain
Uncovering your pain’s secret communication is of great importance. You will identify and personally connect with your pain’s triggers, patterns, and themes. You will discover your pain has a personality. You will learn it may like certain people better than others. It may prefer special foods, liquids, and exercise. It may like specific weather conditions, hot and dry or yearn for cold and damp. It might be a big fan of acupuncture or massage. It may lead you into a great relationship with people of similar struggles.
Your pain may be a morning person or an evening person or one that likes to chat all through the night. It might have a favorite season of the year, a favorite holiday! Your pain is the first warning sign that lets you know when your negative thinking has gone too far. It may do many obnoxious things to get your attention. It may even put you on bed rest! Your pain is always the first one to let you know when it does not prefer something as well as when it is happy and at peace with your choices. When you choose to listen and communicate with your pain it will direct you on your path towards success and healing.
What Is Your Pain Telling You?
This question often puzzles and at times frustrates many of my patients. This is where I need to do a little education about pain and the difference between acute and chronic pain. I believe that whenever you experience pain, it’s helpful to ask: What is my pain trying to tell me? Pain is the signal that says something is wrong and you need to find out what is it; you then need to learn how to manage it. Sometimes it can be difficult if not impossible to pinpoint the pain generator, and as human beings we want to know why something is happening and we want to know “right now.” But when we are in pain the more important question is: What can I do right now to manage my pain in a healthy way that supports me physically, emotionally and spiritually? The answer will be different for each person.
Exploring the Difference Between Pain and Suffering
But what if you can’t answer that question because your chronic pain has become unmanageable, no matter what you try? This brings us to a discussion of pain versus suffering. The psychological meaning that you assign to a physical pain signal will determine whether you simply feel pain (Ouch, this hurts!) or experience suffering (This pain is awful and will just keep getting worse; this is terrible and why is it happening to me!). Although pain and suffering are often used interchangeably, there is an important distinction that needs to be made. Pain is a physical sensation, a warning signal telling you that something is going on in your body. Suffering results from the meaning or interpretation your brain assigns to the pain signal.
Many people believe that: I shouldn’t have pain! Or because I have pain and I’m having trouble managing my pain, there must be something wrong with me. A big step toward effective chronic pain management occurs when you can reduce your level of suffering by identifying and changing your thinking and beliefs about your pain, which in turn can decrease your stress and overall suffering. Because of the two parts—pain and suffering—chronic pain management must also have two components: physical and psychological. The way you sense or experience pain—its intensity and duration—will affect how well you are able to manage it. Thus the need to learn what your pain is telling you!
To request the remainder of this article, please connect with me at drgrinstead@yahoo.com.

A Spiritual Warrior Journey of Hope and Healing Part One
My Story of Learning To Live Life Without Armor
As I achieved 39 years in recovery from alcohol and pain pills and 38 years of living with chronic pain, I knew it was time to look back. My hope is that this article helps others to see that no matter what adversity or overwhelming life situations occur, we have a choice to face and thrive despite them or feel victimized by them.
In the early 1980’s I was dealt a major life blow that many people living with chronic pain may be able to understand. A construction accident left me without my livelihood and robbed me of a new career as a Karate instructor. In my mind life was over, and I seriously considered ending it. But I realized through the love and support of friends and several caring healthcare professionals that I wanted more from life than just being a chronic pain statistic. My acceptance process was just the beginning of overcoming adversity to discover opportunities for hope and healing.
The Early Years of My Armor Development
To understand how I overcame adversity, it’s important to share how I developed the self-defeating coping strategies and defenses that helped me survive. These defenses, or what I’m calling armor, helped to protect me from several painful realities. For the first 28 years of my life I didn’t even realize I was “Armored Up” and I mistakenly believed this armor would keep me safe. I was trapped, and I didn’t even know it. Today I understand this psychological armor helped me live through significant childhood trauma. I hope my story will help you to identify any protective armor you might be wearing that does not serve you well anymore.
My path has been one of progress, not perfection, as my old armor can still be triggered even after almost 40 years of being on my Spiritual Warrior Journey. The difference today is that I am much more aware, catch it sooner and make proactive amends very quickly for any harm I may have caused while armored up – especially because when I get defensive, I can become very offensive.
I believe too many people in our culture are “Armored Up” and convinced they must protect themselves. The most vulnerable and powerful aspects of what makes them unique and beautiful are hidden from themselves and others – they don’t have access to their empathy, compassion and connection that makes an extraordinary quality of life possible. I have observed many people suffering with chronic pain who are the most armored up of all. Over the years I have learned to replace my armor and offensive weapons of anger and violence with Spiritual Warrior Values, Principles and Practices, and so can you!
Daddy Said Real Men Don’t Cry – But They Really Do
An early decision I made at five years old led to my first suit of armor. I was on an exciting fishing trip in the Colorado Rockies with my Daddy and his buddies at a place called Pauline Creek, close to Gunnison Colorado. As the oldest of four boys (Mom eventually had 9), this was a very special occasion for me. I was having such a great time and finally getting the attention from Daddy I craved. I was running and laughing like a maniac as one of Daddy’s buddies chased me with a snowball. In my attempt to get away, I jumped off a cliff.
I was down at the bottom of the rock face which seemed impossibly high for a five-year-old, crying and holding my sprained ankle. Daddy rushed over and I felt relieved as he checked my ankle, but his next words stunned, shamed and paralyzed me, “You’re not hurt that bad so quit crying or I’ll give you something to cry about.” His next comment solidified my decision about vulnerability, “In this world you have to be tough Stevie – real men don’t cry.”
The decision I made as a result informed all my choices: I will never ever risk sharing my pain again – physical or emotional – because I needto be a real man and make my Daddy proud. I started to build my first suit of armor and began hiding who I was, what I felt and what I needed. I reinforced it over the next twenty-five years. My Armor started out as a hardened leather body suit that I mistakenly believed was protecting me, but I didn’t see the barrier I was building between me and other people.
I wonder how many of you reading this can identify with similar circumstances and the decisions I made. Situations, words, people, and actions may be different, but most people in our society receive similar messages from the day they are born about the need to be tough, safe and self-resilient, not trusting anyone with the truth. Self-defeating decisions are often made as a result of interpretations about a perceived hostile environment.
Let me be very clear here; these early defenses do help us survive very toxic situations. I would never suggest anyone drop their armor without having something in place that will serve them in a healthier way, such as Spiritual Values, Principles and Practices.
To request the remainder of this article, please connect with me at drgrinstead@yahoo.com

A Spiritual Warrior Journey of Hope and Healing Part Two
Hitting Bottom And Beginning My Spiritual Warrior Journey
Hitting bottom is a term people use in the recovery community, but there are also some dangerous beliefs about that really means. Sometimes people think they must lose everyone and everything they hold dear before they can start again. Others believe it’s the damage they do to their bodies or mind. And for many it’s experiencing the deep shame of failing despite their best intentions. That’s how my bottom was for me.
At twenty-nine I decided to learn how to live my life without alcohol and pain pills; what I then mistakenly believed to be the most indispensable component that helped me to maintain my armor. But I had an intense desire to stop because of my commitment to Karate and a spiritual life. So, I promised my daughter, myself and my Karate Sensei Kim that I would never drink alcohol or use pain pills again. I believed, as any good Marine would, that self-will, my Karate practice and military discipline would see me through.
It was a year later on January 22, 1981, that I experienced the second worst moment of my life – both emotionally and spiritually. I used pain pills despite my best intentions and hit my real bottom. I felt so ashamed over having failed and disappointed everyone who I made promises to.
I’ll never forget that night. I was in my living room on my knees crying and feeling intense shame and a sense of total failure when the song “Help” by the Beatles came on. I heard it in a completely different way that night. I sang along and addressed this musical prayer to my Higher Power, begging for spiritual help – and boy did I receive it! I felt inspired and reached out to my spiritual mentor the very next day. That was a significant turning point for me – I truly began the search to find the Spiritual Values, Principles and Practices that I would live the rest of my life by.
In 1982, at age thirty-two, clean and sober with a black belt in Karate, I was getting ready to leave my life as a construction electrician and open my own Dojo. A work accident led to what became my darkest hour as a Spiritual Warrior. I was injured on a job and could no longer do the work that I believed made me a real man but more importantly, to practice the Martial Art I truly loved.
I was paralyzed from the waist down for almost two weeks and fell into a very deep depression – my pain was unrelenting and became a chronic condition. I believed my life was over; I felt hopeless, helpless and began to suffer with my pain. I experienced a place so dark that I came to call it the Chronic Pain Trance, where dying seemed to be my only choice. That was the lowest point of my life and the place where I started to let go of everything I had learned on my spiritual recovery journey. I took on aspects of my old armor again, and I almost didn’t survive.
Fortunately, with the love of friends, caring healthcare providers, and the healthier part of me, I knew there was a better way. I was open to help and made the decision to live. This is where I began my journey of hope and healing as a true Spiritual Warrior so that I might find real freedom from my suffering. I stopped depending on the old armor and started to develop and use new Spiritual Values, Principles, and Practices. I learned how to be vulnerable, humble and teachable.
My journey included psychotherapy with an awesome trauma therapist while at the same time working in physical therapy and hydrotherapy. I went from not being able to walk to taking 3-5-mile hikes. I was on the way now. At the same time, I also started expanding my Spiritual Journey by attending many Spiritual retreats and I spent a large amount of time at the Esalen Institute for even more Spiritual and Psychological healing.
My journey also included working with a Vocational Rehabilitation Counselor who discovered that I had great people skills so and encouraged me to enroll at University of California Santa Cruz (UCSC) and complete two years in Human Counseling and concurrently completing the USCS Certified Alcohol and Drug Studies Program. I had now transitioned into becoming a healthcare provider as a Certified Alcohol and Drug Counselor.
To request the remainder of this article, please connect with me at drgrinstead@yahoo.com

The New Rules for Treating Chronic Pain
Addiction-Free Solutions In The Era of Opioid Crisis
Prolog
This past year of COVID-19 has changed the face of healthcare in many ways; some positive and some extremely negative. There have been many casualties of COVID-19 above and beyond those living and dying with the exposure to this disease. Some of those casualties are people with chronic pain and coexisting disorders including addiction, PTSD, Depression, Anxiety and many other mental health problems. The other noted victims are people dying from Opiate/Opioid overdoses, in many cases due to not receiving adequate treatment interventions by their healthcare providers. Because of COVID-19 we have lost focus on the so-called Opioid Epidemic. This article outlines some of the overwhelming problems that led to what I am calling the Opioid and Chronic Pain Syndemic. Then I outline the need for implementing a synergistic solution that needs to include everyone. I am also including two case study examples to demonstrate the need and effectiveness of an Addiction-Free Pain Management® synergistic treatment solution.
Understanding the Problem is Crucial to Finding the Solution
I believe there is much more than an opioid crisis or epidemic. It is not an epidemic, rather it is a Syndemic. What I mean by that is it’s a perfect storm of over prescribing opioids, mismanaged chronic pain by depending only on the traditional bio-medical model and untreated mental health disorders. What we need to focus on is identifying the synergistic nature of the problem and the need to implement a synergistic treatment solution that helps heal the whole person – Biological, Psychological, Family/Social and Spiritual. A true Body-Mind-Spirit Approach.
There is also a strong political and financial component to our current problem that Harry Nelson outlines so well in his book The United States of Opioids: A Prescription For Liberating A Nation In Pain. Also, in his book Dreamland: The True Tale of America's Opiate Epidemic, Sam Quinones also covers some of the financial and political precursors to our current problem.
In addition, many people believe what underlies this crisis is a severe deficit in coping skills for those who are suffering with chronic pain and coexisting mental health disorders including substance use disorders. Combine these poor coping skills with misinformation from leading medical prescribers using opioids for chronic pain, and we see addiction from prescription opioids has increased over 1,000 percent between 2012 and 2016. The Center For Disease Control (CDC) posted an update on December 16, 2016 with some other staggering statistics:
- Over 1,000 people a day are being treated for prescription opioid overdose incidents with the three most common being Methadone, Oxycodone/OxyContin, and Hydrocodone.
- As many as 91 people a day are dying from prescription opioid overdose events.
- Between 1999 and 2015 there were over 183,000 deaths directly related to prescription opiates.
- Finally, in 2014 over 2 Million Americans experienced prescription medication misuse, abuse, pseudoaddiction or addiction. Many say this is an opioid epidemic.
The other coexisting epidemic noted is chronic pain. Chronic pain management is a serious health crisis facing the world today. In fact, in the well-publicized June 2011 White Paper The Institute of Medicine (IOM) stated that as many as 116 million people were experiencing chronic pain; the cost of managing it in the United States alone is over $635 Billion per year in direct medical costs and lost productivity. As I write this today the problem continues to worsen.
When a person who is undergoing chronic pain management, they are also experiencing other co-existing disorders, such as medication abuse or even addiction to prescription pain medication and psychological disorders, the problem reaches even more epidemic proportions. Every week in the media there are reports about the problematic use and/or abuse of prescription drugs being used in the treatment of chronic pain. The numbers of people impacted are staggering.
So what is the source of the so-called Opioid Epidemic and is there a link to chronic pain? A study posted in the New England Journal of Medicine in March of 2016, reported some interesting numbers in answer to this question.
More than 30 percent of Americans have some form of acute or chronic pain and among older adults; the prevalence of chronic pain is more than 40 percent. In 2014 alone, U.S. retail pharmacies dispensed more than 245 million prescriptions for opioid pain relievers. Opioids are widely diverted and improperly used. In addition, many physicians admit that they are not confident about how to prescribe opioids safely.
This report went on to state that more than a third (37 percent) of the 44,000 drug-overdose deaths that were reported in 2013 were attributable to pharmaceutical opioids while Heroin accounted for an additional 19 percent. There was also a parallel increase in the rate of opioid addiction, affecting approximately 2.5 million adults in 2014.
Alterations in brain functioning from living with chronic pain explains why long-term pain leads to cognitive deficits, as well as anxiety and depressive disorders. Emotional and cognitive deficits sometimes begin long after the onset of pain. Long-term pain may be detrimental to the brain and decrease the ability to endogenously control the pain and frequently lead to many comorbidities. (Neuroscience: 14: July 2013).
Unfortunately, the research numbers do not come close to capturing the true cost of the human pain and suffering experienced by those individuals with addiction whose pain condition is either under-treated or mistreated. When you add in the impact on families, friends and communities, it becomes even more devastating.
On September 16, 2016, Time Magazine came out with a report about why chronic pain patients turned to Heroin and the catastrophic results. The report stated that Heroin-related overdoses have almost quadrupled over the last decade in the U.S., leading to more than 10,000 deaths in 2014 alone. Heroin is being laced with Fentanyl and Carfentanil, two powerful synthetic opiates that are linked to a string of overdoses in the Midwest and Appalachia. In addition, since that time it has spread all across the nation.
A CNN Report on June 2, 2016 stated that today’s typical heroin addict starts using at age 23, is more likely to live in the affluent suburbs and was likely unwittingly led to heroin through the use of painkillers prescribed by his or her doctor. While heroin is illicit and opioid pills such as oxycontin are FDA-approved, each is derived from the poppy plant. Their chemical structures are highly similar, and they bind to the same group of receptors in the brain.
The FAIR Health, Inc. White Paper, in September 2016, covered the negative impact of the Opioid epidemic on healthcare. It showed the cost for opioid-related treatment rose over 1,000 percent from 2011 to 2015. It also stated that in 2015 Private Payers’ average costs for a patient diagnosed with opioid abuse or dependence were more than 550 percent higher than the per-patient average cost based on all patients’ claims and Emergency Room visits made up a large percentage of these costs.
The FAIR Health report went on to state that the bio-medical approach alone clearly doesn’t work for this poor outcome subset of chronic pain patients with coexisting disorder who end up over-utilizing the healthcare system and experience disappointing outcomes. So what does work? Now we are ready to get out of the problem and into the solution.
Investigating Potential Synergistic Solutions
In looking at potential solutions I’d like to review the cases of two of my former patients; the first, Patient One, is an excellent example of what can happen when a chronic pain condition is not managed appropriately and treatment depends only on medication-one part of the Biomedical approach.
To request the remainder of this article, please connect with me at drgrinstead@yahoo.com.
Thank You Adversity Available Now!
Free: Prologue, Table of Contents, Forward & First Chapter
Copyright © 2026 Grinstead Consulting & Training - All Rights Reserved.- 916-893-3155 - drgrinstead@yahoo.com